Surgical treatment of acquired heart defects
Aortic valve disease
Surgical treatment of patients with aortic insufficiency is indicated in all symptomatic patients in NYHA functional class II or higher with ejection fraction >20–30% or end-systolic diameter <55 mm. End-diastolic diameter approaching 70 mm is an additional indicator. Patients with more severe damage to left ventricular contractile function have a significantly higher risk of surgery and postoperative mortality. Aortic valve replacement is indicated in all patients with symptomatic aortic stenosis and in asymptomatic patients with high transvalvular pressure gradient (> 60 mm Hg), orifice area ≤0.6 cm2, coronary or other valve pathology, before left ventricular decompensation develops.
 |
 |
 |
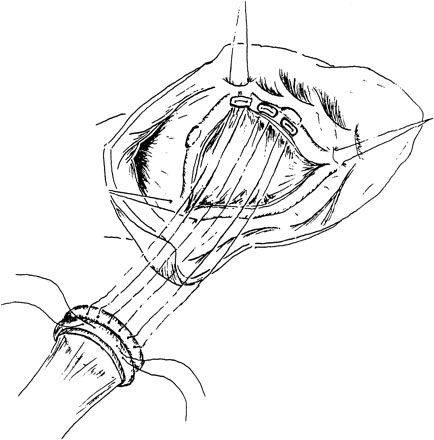
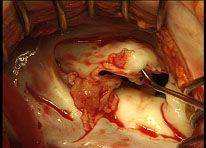
Surgical correction of aortic malformation is performed by means of its prosthetics with mechanical, biological skeletal, and frameless prostheses or cryopreserved allografts.
 |
In some patients it is possible to perform aortic valve reconstruction. In cases of narrow aortic rings aortic root plasty with biological material is performed to achieve optimal hemodynamics. The surgeries are performed using both standard and minimally invasive access.
Mitral valve disease
The indications for surgery in mitral stenosis are determined by the area of the left atrioventricular orifice. Mitral stenosis with MV area ≤1 cm2 is considered critical. In physically active patients or patients with high body weight, an orifice narrowing of 1.2 cm2 may also be critical. Thus, the indication for surgery in patients with mitral stenosis is decreased MV area <1.5 cm2 and NYHA functional class II or higher.
The indications for surgery in mitral insufficiency are effective regurgitation orifice size >20 mm2, II and more degree of regurgitation and II-III NYHA functional class. Surgical treatment of mitral insufficiency should be performed before ESVI reaches 40–50 mL/m2, as its increase ≥60 mL/m2 suggests an unfavorable prognosis.
 |
 |
 |
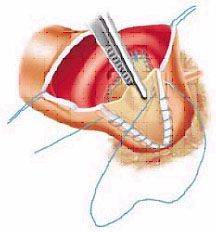
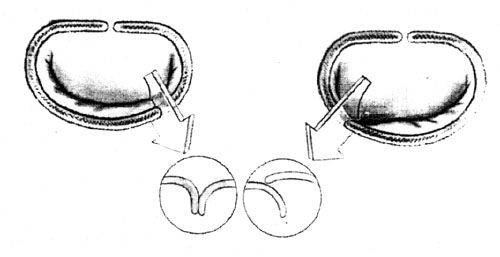
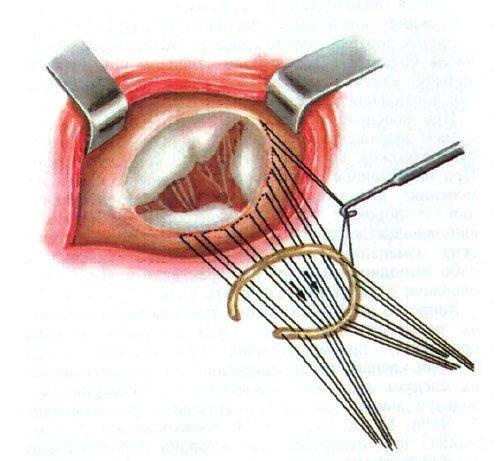
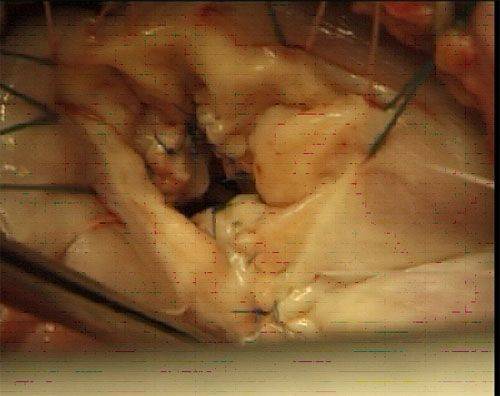
Surgical correction of mitral defect is performed by means of its prosthetics with artificial mechanical, and biological prostheses.
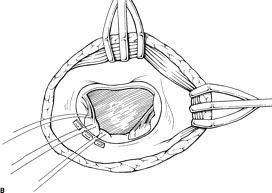 |
When implanting prostheses in patients with severe heart failure, preservation of natural chordal apparatus or implantation of artificial polytetrafluoroethylene chords is mandatory.
 |
 |
 |
 |
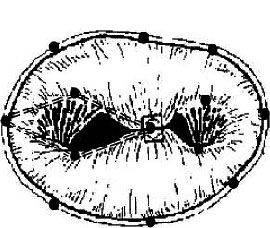 |
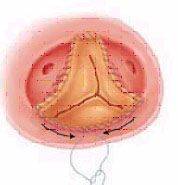
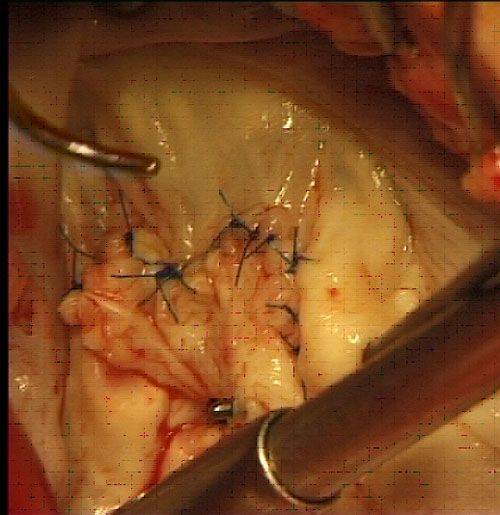
In 30–40% of patients it is possible to perform reconstructive surgery on the mitral valve. Various methods of reconstruction are used for this purpose: annuloplasty on hard and soft rings, resection of the leaflets, implantation of artificial chords, "edge-to-edge" plasty. Restoration of normal mitral valve function in the majority of patients subsequently does not require lifelong anticoagulant therapy.
 |
Mitral valve surgery is performed both with standard sternotomy, and right sided minithoracotomy.
Tricuspid valve disease
The indication for surgery in tricuspid valve stenosis is the effective orifice area <1.5 cm2, and in insufficiency — regurgitation of blood into the right atrium of II-III degree. When choosing the method of tricuspid valve disease treatment, the patient's predictors of residual pulmonary hypertension are taken into account: PAP >50 mm Hg, RV wall thickness > 7 mm, LV diameter >55 mm, RVEF < 30%.
 |
Annuloplasty is the main method of relative tricuspid valve insufficiency correction. Methods of tricuspid valve ring diameter reduction include cystoplasty and the use of rigid or flexible corrective rings. In some cases, if corrective surgery cannot be performed, valve bioprosthesis is used.
 |
Infectious and prosthetic endocarditis
The etiology of infective endocarditis has changed significantly due to the active use of antibiotics worldwide. Staphylococci and gram-negative flora, as well as fungal infection, now play a major role.
 |
From the surgical point of view in the pathogenesis of infectious endocarditis the fact of rapid destruction of the cardiac valve apparatus is of the greatest concern. This leads to a catastrophic increase in heart failure incidence, since the myocardium has no time to adapt to the rapid violation of hemodynamics.
The need for surgical treatment arises, as a rule, in the development of "complicated infectious endocarditis": changes in hemodynamic status; persistence and prevalence of infection; development of metastatic foci of infection; systemic emboli. In these cases, surgical treatment is more successful than the therapeutic approach.
The main problem of surgical treatment is the prevention of recurrence of infection and the development of prosthetic endocarditis. The basis for the choice of tactics is anatomical changes detected on the operating table: the degree of fibrous ring and surrounding tissues damage, as well as the presence of vegetations, abscesses, fistulas, prosthetic tears. Of particular importance in recent years are reconstructive surgeries, especially when the mitral or tricuspid valves are affected by endocarditis. To replace valve defects after surgical treatment we use plasty with own tissues, autologous or xenopericardium.
 |
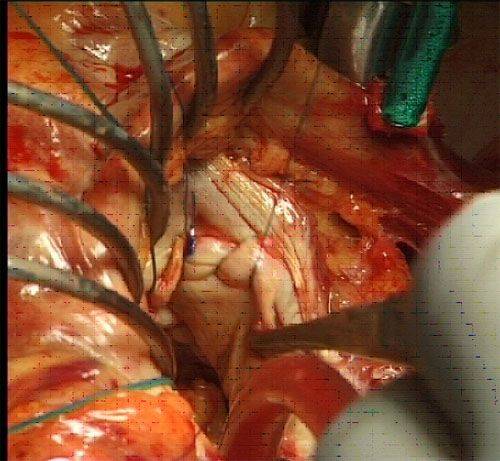 |
 |
Artificial heart valves
Currently, the Center uses mechanical, and biological artificial valves, as well as allografts.
Mechanical prostheses
 |
 |
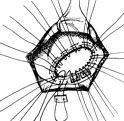
Two modifications of bicuspid artificial heart valves are developed and used in the Center: PLANIKS-T and PLANIKS-E. The difference of design of the last version of native bicuspid heart artificial valve from the previous model is that the body of prosthesis is covered by titanium oxide, providing high wear resistance and biological inertness. The big height of the swivel mechanism prevents the leaves from jamming by the heart tissue and has allowed to increase the opening angle of the leaves up to 90◦.
Biological prostheses
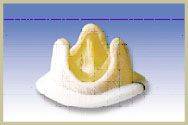 |
 |
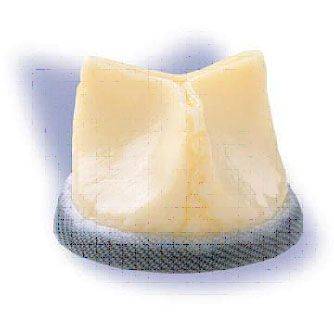 |
 |
 |
 |
The leaflets of the prosthesis are formed of biological tissues: xeno-aortic valve, pericardial valve. Two types of bioprostheses are used: framed (the biological tissue is fixed on a rigid or flexible frame) and frameless.
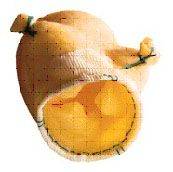
Allografts
 |
A modern trend in the surgical treatment of valve lesions is the use of cryopreserved allografts. In recent years, the emergence of modern cryogenic technology has made it possible to create conditions for long-term preservation of viability of biological objects, which ensures their normal function in the body after implantation.









