Endovenous laser ablation (EVLA)
Varicose disease is a serious disorder which, if no prevention measures are taken, progresses with time and may contribute to the development of complications including stasis ulcers and thrombophlebitis. When the thrombus is localized in a major vein, i.e.there is a high risk of the detachment that is perilous for patients to the extent that there might be a fatal outcome. Therefore, permanent monitoring of venous condition and timely management are a top priority.
First signs of varicose disease are not apparent in majority of cases, but there is a discomfort including fatigue in legs, ankle and feet oedema, lower leg muscle seizures are possible in the late evening or at night. More often, patients relate these symptoms with excessive tiredness, overloads and “simply a difficult week” thing, but it seems already necessary to consult a doctor and take measures to prevent disease progression. If there are disorders in saphenopopliteal junctions, major and minor venous stem valve and perforating veins, in most cases it causes protuberant varicosities and chronic varicose failure (CVF).
Telangiectasis or ‘spiders’, and reticular varicose or thin percutaneous vein extension do not give rise to patients complaints, except for a minor cosmetic discomfort, mostly in women, but in the presence of these symptoms, one should take measures instead of waiting until this esthetic inconvenience becomes physically discomfortable.
The treatment of varisoce disease should be multifaceted and include medical and compression therapies together with surgery – venectomy or phlebectomy. More novel and effective methods are being constantly developed. Unlike conventional phlebectomy that makes marks on legs and makes postoperation and rehabilitation period longer, endovenous laser ablation (EVLA) is performed in outpatient settings and requires no in-hospital stay (in-hospital stay lasts 3-5 hours including procedure), and then the patient can return to their daily activities. During the laser operation, the risk of nerve and lymph node injury is reduced and no marks are left, and protuberant varicosities are removed via punctures of several millimeters. There is also a minimal risk of complications as well as the risk of relapses compared to conventional operation on veins. After surgery, patients should wear compression stockings (during 3 weeks). The procedure of laser vein coagulation currently used produces excellent results and cosmetic effects.
The first visit to a specialist includes clinical examination, US study of lower limbs and specialist advice. The US examination assesses the extent of permeability of deep and surface veins, functioning of venous valves, analyzes the presence/absence of reflux (regurgitation) and the condition of perforating veins. If a significant reflux in subcutaneous veins has been found, endovenous laser ablation is recommended.

The Centre performs endovenous laser ablation using state-of-the-art equipment used worldwide. Ceralas E system by Biolitec AG, Germany, utilizes Radial ElVeS Painless (Biolitec AG, Germany) technology using disposable laser light guides ELVeS Radial and Radial 2Ring and laser apparatus (generator) with wave frequency of 1470nm (laser apparatus utilizes special technologies preventing second use of laser light guides). The tip of the light guide features a special microlens that provides scattering of radiation and its even distribution around the working area of the light guide, and finally it produces optimal effect when sealing veins of any diameter. This feature of laser radiation scattering allows for the effective injury management and almost a 100% reliable venous sealing. Advantages of the procedure also include low pain level after operation and small mild hematomas.
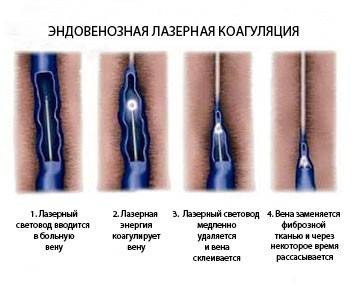
The light guide inside a vessel is used as follows:
Anaesthesia: during the procedure, a tumescent anaesthesia, i.e a local analgesia, after which along the vein a specialized cold anesthetic solution is introduced which allows for a certina buffer around the injury reducing blood fullness in the vein and lumen narrowing facilitating the procedure.
US control: US utilizes tumescent anesthesia and the puncture of the vein in which a laser light guide is inserted.

Apparatus functioning: a specialist defines and sets the values of the energy level needed to perform the procedure in any individual case. The light guide is connected to the apparatus and when it is located in the point of interest, the laser coagulation begins, and the light guide is gradually leaving the vein. Surgery: the main step is often 20-30 minutes long. If any lateral protuberant varicosities are present, a mini-phlebectomy is performed (Varady’s operation), or protuberant lateral inflow sclerotherapy. These methods may be used as one-step procedure utilized stem EVLA, or as a second-stage after 3-4 months (stem coagulation results in reduced lateral inflows). After procedure, aseptic dressing is applied and ribbed tights or second- degree compression stockings are put on. In 30-40 minutes after procedure, the patient may leave the hospital having preliminary received a specialist’s advice.









